Policymakers and clinician consortia have identified low value care, defined as health care services that provide negligible clinical benefit to the patient when provided, as one way to curb excessive and inefficient medical spending. A previous HCCI report found that 18% of people with employer-sponsored insurance in 2019 received at least one low-value service, which corresponded to 2.6% of overall health care spending. Additionally, more than 60 percent of low-value care use and spending was concentrated in just 7 services.
In 2022, the Research Consortium for Health Care Value Assessment introduced the concept of “no value care.” A step beyond low value care, for no value care, there are no circumstances under which a service or procedure would be clinically beneficial to patients, and, in some cases, such care could cause patient harm. To date, there is not a universal definition on how to identify no value care services. The definitions of no value care have varied, including defining it as USPTSF grade D services to identifying a subset of Choosing Wisely services. Most definitions rely on clinical factors, such as whether a patient is symptomatic or at increased risk, in determining whether a particular service is of no value.
In this brief, we build on previous work to identify “no value care” among the employer-sponsored insurance population. We limited our analyses to three “no value care” services where administrative claims data contain sufficient clinical and demographic elements to reasonably identify “no value care”: Vitamin D tests, arthroscopic knee surgeries for osteoarthritis, and prostate specific antigen (PSA) tests. See Methods section for more details.
Use of Vitamin D Screening, Arthroscopic Knee Surgeries for Osteoarthritis, and PSA Testing
Prior to 2020, utilization of Vitamin D screening among people with employer-sponsored insurance had been decreasing. Some of the lower use in 2020 likely is related to an overall decrease in use of health care services in that year associated with the COVID-19 pandemic. From 2020 to 2021, our data show an increase in the rates of vitamin D screenings (from 108.83 per 1,000 to 131.20 per 1,000). The 2021 rate is higher than the 2019 and 2018 rates, suggesting that the increase is likely more than a return to pre-pandemic utilization patterns. The rate of Vitamin D screening remained at levels slightly higher than pre-pandemic years in 2022.
Vitamin D screening among those with Traditional Medicare also saw a decline in 2020 and resurgence in 2021 and 2022. Rates of vitamin D screening were hovering around 280 per 1,000 in 2018 and 2019 before dropping 6% to 264.60 per 1,000 in 2020. By 2022, rates of Vitamin D screening increased to 312.28 per 1,000.
As expected, rates of arthroscopic knee surgery for osteoarthritis were dramatically lower than of Vitamin D screening. The rate of arthroscopic knee surgery decreased steadily from 2018 to 2022 (0.54 per 1,000 to 0.35 per 1,000). As with Vitamin D tests, 2019 to 2020 saw the largest decrease in use over the five-year period. Unlike Vitamin D tests, the rate of use of arthroscopic knee surgery for osteoarthritis did not rebound in 2021. It stayed constant from 2020 to 2021 and declined again in 2022. Among those with Traditional Medicare, we see a similar steady decline from 2018 to 2022 (0.48 per 1,000 to 0.31 per 1,0000).
PSA testing was only assessed among Traditional Medicare since these tests are generally considered clinically beneficial for the younger employer-sponsored insurance population (<65 years), and limitations in the ESI data do not allow identification of the specific age criteria designed to identify no value PSA tests. PSA testing among those with Traditional Medicare increased from 2018 to 2022, aside from a small (less than 5%) dip in 2020. In 2018, the rate of PSA testing was approximately 201 per 1,000, and it increased by almost 13% to about 227 per 1,000 in 2022. (See Appendix.)
Spending on Vitamin D Screening, Arthroscopic Knee Surgeries for Osteoarthritis, and PSA Tests
Spending on Vitamin D screenings accounted for approximately $5 billion over the five-year period between 2018 and 2022. Of that spending, $3.5 billion was among people with ESI, and $1.5 billion was among people enrolled in Traditional Medicare. Over the same five-year period, spending on arthroscopic knee surgeries for osteoarthritis totaled $2.5 billion. Most of that spending ($2.3 billion) was concentrated among the ESI population with about $195 million in Medicare fee-for-service spending. Spending on PSA testing from 2018-2022 was about $750 million all in the Medicare population (Figure 1).
In 2022 alone, Vitamin D spending was nearly $1 billion ($709 million in ESI and $287 million in Medicare). Spending on arthroscopic knee surgery for osteoarthritis in that year was nearly $420 million. Most of that spending was among people enrolled in ESI ($389 million) with a smaller amount (approximately $30 million) on people with Medicare. In 2022, spending on PSA tests in Traditional Medicare was $143 million (Figure 2). A data table is available in the Appendix.
Identifying No Value Vitamin D Screening, Arthroscopic Knee Surgeries for Osteoarthritis, and PSA Testing
As shown in Table 1, among the three no-value care services we studied, arthroscopic knee surgeries for people with ESI had the highest percentage of services that were no value. In 2022, approximately 45% of arthroscopic knee surgeries for osteoarthritis met the criteria of no value care. Vitamin D screening in Traditional Medicare had the lowest proportion of services that were considered no value. In 2022, only 4% of Vitamin D screenings were likely no value. Vitamin D screening among people with ESI (23%), PSA testing (21%), and arthroscopic knee surgeries (18%) among people in Traditional Medicare had similar proportions of no-value services in 2022.
Overall, the data do not reveal consistent patterns of no-value care service use. The lone similarity is that, in both the ESI and Traditional Medicare populations, there is a higher portion of arthroscopic knee surgeries that are no value than Vitamin D screenings. Otherwise, each population and service seems to follow a slightly different pattern. The proportion of Vitamin D screenings that were of no value decreased between 2018 and 2022 (31% to 23%) among the ESI population but remained relatively flat at 4% among people with Traditional Medicare.
Rates of no-value arthroscopic knee surgery increased slightly from 2018-2022 (42% to 45%) among people with ESI. Among the Traditional Medicare population, in contrast, the percentage of arthroscopic knee surgeries that are no value decreased from 25% in 2018 to 18% in 2022.
The percentage of PSA tests that were no value were fairly flat over the five-year period staying at about 20%, though there was a slight increase in 2022.
Figure 3 shows the proportion of spending on these two services that can be attributed to no value care among those with employer sponsored insurance. The proportion of spending follows closely the pattern of utilization. For example, our data suggest that, among the ESI population, 24% of spending on Vitamin D screening in 2022 is attributable to no value care, down from 31% in 2018. Among Medicare enrollees, the proportion of spending was relatively flat at 4% for most years of the five-year period. As with use, the proportion of spending on knee surgeries attributable to no value care was higher than Vitamin D screening. As with utilization patterns, the proportion of spending on no-value services declined for ESI Vitamin D screening and Traditional Medicare arthroscopic knee surgeries. The percentage of spending on no-value arthroscopic knee surgeries among people with ESI increased from 2018 to 2022.
Provider rates of no value care in ESI differ by specialties in Vitamin D Screenings
To determine whether certain providers were more likely to conduct no value care, we looked at whether higher rates of no value services in our data were concentrated among certain specialties.
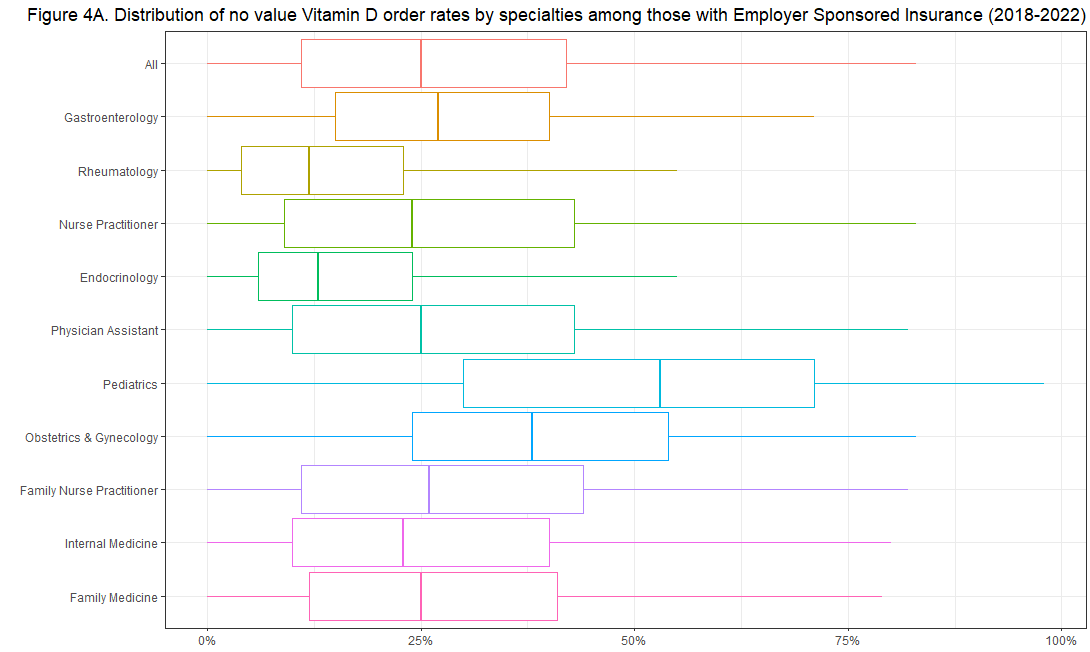
We estimate that, among all the providers we identified as ordering Vitamin D screenings for the ESI population, the median ordering rate of no value Vitamin D screening was 25% (Figure 4A).
Although the proportion of Vitamin D Screenings that were of no value was fairly consistent across provider specialty, we do observe some variation. For example, it appears that pediatricians and ob-gyns had higher rates of no-value Vitamin D Screenings compared to all providers with median rates of 53% and 38%, respectively. This could reflect how applicable definitions of no value Vitamin D Screenings are to children and women as much as any insight about practice patterns among these specialties.
In contrast, we observe that the rate of no-value of Vitamin D screening among endocrinology and rheumatology providers is lower than other specialties. The median proportion of no-value tests is 13% among endocrinologists and 12% among rheumatologists. These providers may have lower rates of no-values screenings since they care for more patients with conditions that clinically justify Vitamin D screenings, such as thyroid disorders and osteoporosis. The low overall rate of no value Vitamin D screenings among those with Traditional Medicare is reflected in the distribution by provider specialty – the median ordering rate was 0% among providers in the most common specialties
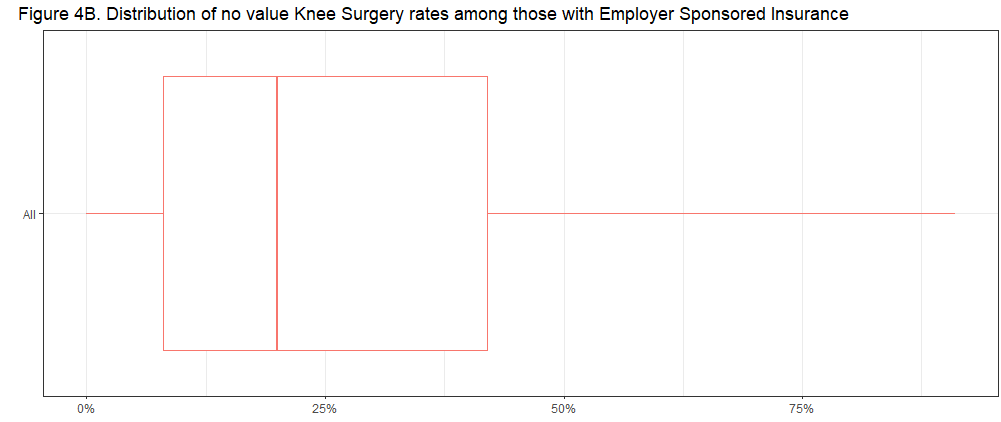
Due to the specialized nature of knee surgeries, we did not look at the distribution of no value services by provider specialty. Among the surgeons performing arthroscopic knee surgeries for osteoarthritis for patients with employer sponsored insurance, we found that 20% of the surgeries performed did not have evidence of clinical benefit to the patients (Figure 4B). Among those with Traditional Medicare, we found the median surgeon had low rates (0%) of no value surgeries.
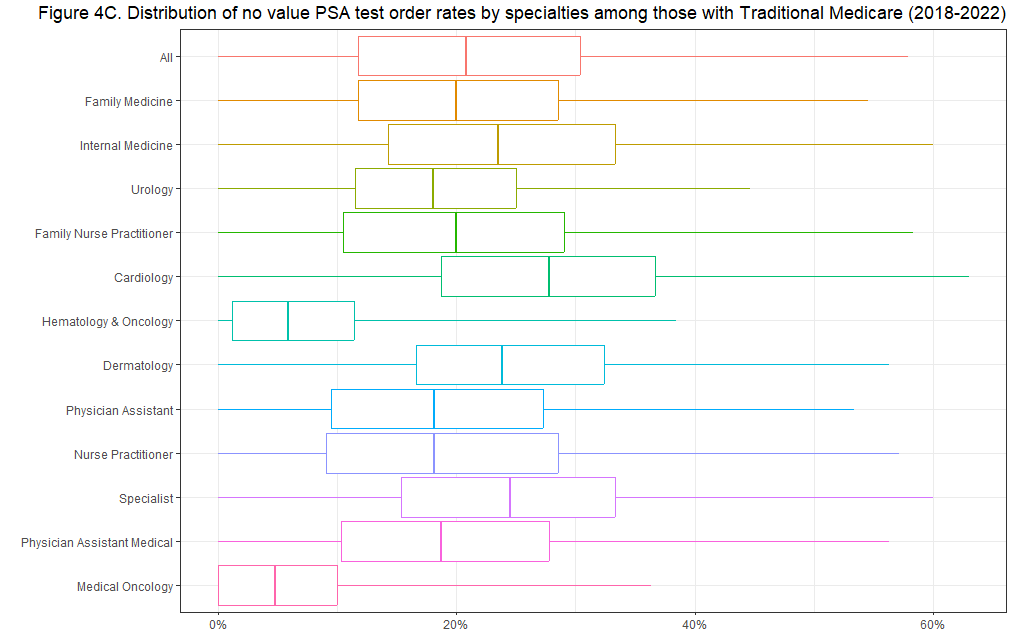
Among providers we identified in Traditional Medicare ordering PSA tests, we estimate the median ordering rate of no value PSA testing was just over 20% (Figure 4C). The most common specialties, Family Medicine and Internal Medicine, have a median rate of 20% and 24% respectively. In contrast, we see substantially lower rates among Hematology & Oncology and Medical Oncology provider specialties with median rates of 6% and 5% respectively. These providers may have lower rates of no-value screenings since they are caring for patients with cancer, in which case PSA testing may be warranted in older patients.
Opportunities to Address No Value Care, but It Can be Challenging to Identify
In this brief, we calculated the prevalence and spending among a subset of “no value care” services between 2018 and 2022 among the employer-sponsored insurance and Traditional Medicare populations. Vitamin D Screening in administrative claims accounted for nearly $708 million in ESI and $312 million in Traditional Medicare spending in 2022. In that year, we estimate that 23% of all Vitamin D Screenings had no evidence of clinical benefit in administrative claims data among those with Employer Sponsored Insurance, much higher than the estimated 4% no value tests among those with Traditional Medicare, The prevalence of arthroscopic knee surgeries for osteoarthritis amounted to $389 million in ESI and $30 million Traditional Medicare spending in 2022.
Our analysis focused just on these three services and, accordingly, does not speak to the prevalence of “no value care” in the employer-sponsored insurance and Traditional Medicare population broadly. Due to absence of clinical and health care operation data elements, we are not able to identify and measure most “no value care” or related challenges, such as medical mistakes, preventable infections, lack of care coordination, and lack of access to care.
Appendix
Methods
Arthroscopic surgery for knee osteoarthritis
- Arthroscopic knee surgeries were identified using facility and professional claims during the calendar year. Surgeries were restricted to those that contained diagnosis codes for osteoarthritis on the surgery claim. Spending associated with arthroscopic knee surgeries for osteoarthritis included all incurred medical costs on the day of surgery and does not include any follow up care cascades.
- Overall rates and spending of arthroscopic knee surgeries for osteoarthritis are presented among 1,000 enrollees. ESI calculations are weighted to the total ESI population, and Traditional Medicare calculations are performed on 100% Fee For Service Medicare data.
- The no-value algorithm for arthroscopic knee surgery for osteoarthritis, including surgery procedure codes and diagnosis codes, was adapted from Do et al (2022). Knee surgeries were identified as no-value care if there was no evidence of meniscal tears on the surgery claim. Meniscal tears were identified by diagnosis codes.
- Provider analysis: For each surgery we assigned a provider using the most recent evaluation and management service the patient received from the date of surgery to up to 2 weeks prior. We calculated the proportion of surgeries per provider that were identified as no-value and presented the distribution of proportions overall.
Vitamin D Screening
- Vitamin D screenings were identified using facility and professional claims during the calendar year. Spending associated with Vitamin D screenings include only the costs for the test itself and do not include any follow up care cascades.
- Overall rates and spending of Vitamin D screenings are presented among 1,000 enrollees. ESI calculations are weighted to the total ESI population, and traditional Medicare calculations are performed on the 100% Fee For Service Medicare data.
- The no-value algorithm for Vitamin D screening, including procedure codes and diagnosis codes, was adapted from Mafi et al (2017). We required a 1-year lookback period of continuous enrollment to assess patient clinical history that would exclude Vitamin D screenings as having clinical benefit.
- Vitamin D screenings were considered no-value if there was:
- No evidence of certain chronic conditions 1 year prior to testing date
- No evidence of additional risk factors 90 days prior to testing
- No diagnoses for pregnancy and obesity the day of testing
- No diagnoses for falls or traumatic fractures within 1 year prior to testing date
- No diagnoses for Vitamin D disorders or phosphate metabolism 90 days prior to testing date
- Vitamin D screenings were considered no-value if there was:
- Provider analysis: For each Vitamin D Screening test with sufficient continuous enrollment, we assigned a provider using the most recent evaluation and management service the patient received from the date of Vitamin D screening to up to 2 weeks prior to the test. We calculated the proportion of tests per provider that were identified as no-value, and presented the distribution of proportions for the most common provider specialties.
PSA Testing (Traditional Medicare Population only)
- PSA tests were identified using facility and professional claims during the calendar year. Spending associated with PSA tests only includes the costs for the test itself and does not include any follow up care cascades.
- Overall rates and spending of PSA tests are presented among 1,000 enrollees. Traditional Medicare calculations are performed on the 100% Fee For Service Medicare data.
- The no-value algorithm for PSA test was adapted from Mafi et al (2017).
- PSA tests were considered no-value if:
- Beneficiary age 75 with no history of prostate cancer per Chronic Conditions Warehouse first-ever prostate cancer date
- PSA tests were considered no-value if:
- Provider analysis: For each PSA test we assigned a provider using the most recent evaluation and management service the patient received from the date of PSA test to up to 2 weeks prior to the test. We calculated the proportion of tests per provider that were identified as no-value, and presented the distribution of proportions for the most common provider specialties.
References
Do, L.A. et al. (2022) ‘State-level variation in low-value care for commercially insured and Medicare Advantage Populations’, Health Affairs, 41(9), pp. 1281–1290. doi:10.1377/hlthaff.2022.00325.
Mafi, J.N. et al. (2017) ‘Low-cost, high-volume health services contribute the most to unnecessary health spending’, Health Affairs, 36(10), pp. 1701–1704. doi:10.1377/hlthaff.2017.0385.
