Surprise Billing
-
Real World Consequences of the Qualifying Payment Amount in the No Surprises Act
Tags: Surprise Billing Read more: Real World Consequences of the Qualifying Payment Amount in the No Surprises Act
Read more: Real World Consequences of the Qualifying Payment Amount in the No Surprises ActThe United States Congress passed the No Surprises Act last year, offering several protections to consumers. Beginning in 2022, providers can no longer bill patients for more than their insurance’s in-network cost sharing. The law also bans balance billing except in situations where a patient is notified in advance and their written consent is obtained….
-
How common is out-of-network billing?
Tags: Commercially Insured, Emergency Room, Geographic Variation, Mental Health and Substance Use, Out-of-Network, Surprise Billing Read more: How common is out-of-network billing?
Read more: How common is out-of-network billing?Congress is considering legislation to address “surprise bills”, which occur when a person visits an in-network facility, but receives services from a provider that is outside of their insurer’s network. Bills in both the House and Senate include provisions to determine a benchmark rate for out-of-network payments based on what in-network providers of the same…
-
Comparing Commercial and Medicare Rates for Select Anesthesia, Emergency Room, and Radiology Services by State
Tags: Commercially Insured, Emergency Room, Medicare, Physician Spending, Prices, Spending, Surprise Billing Read more: Comparing Commercial and Medicare Rates for Select Anesthesia, Emergency Room, and Radiology Services by State
Read more: Comparing Commercial and Medicare Rates for Select Anesthesia, Emergency Room, and Radiology Services by StateCommittees in both the House and Senate have advanced legislation that includes measures to address “surprise bills.” A surprise bill results when a person unknowingly receives medical care from a provider that is not part of their insurer’s network. Both pieces of legislation set a benchmark for out-of-network payments. Those benchmarks are determined based on…
-
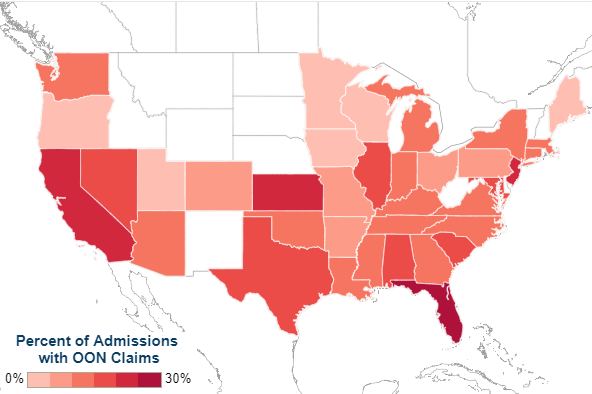
Surprise out-of-network medical bills during in-network hospital admissions varied by state and medical specialty, 2016
Read more: Surprise out-of-network medical bills during in-network hospital admissions varied by state and medical specialty, 2016Out-of-network billing practices have increasingly garnered attention as individuals with commercial health insurance continue to experience “surprise billing.” A surprise medical bill commonly describes a charge to a patient for care delivered by an out-of-network (OON) professional who works within an in-network facility. We used the Health Care Cost Institute’s (HCCI) vast commercial claims database to…